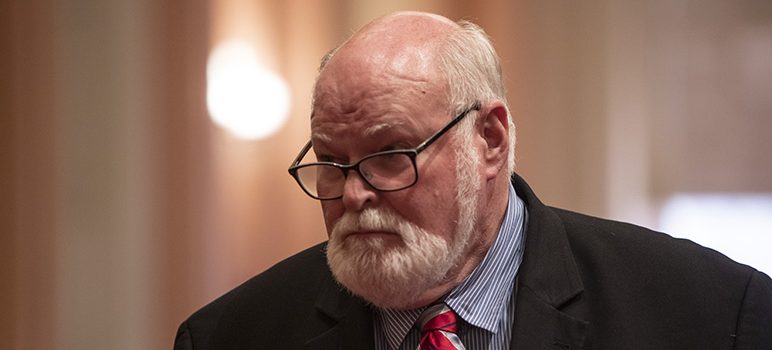
State Sen. Jim Beall is angry.
Four times now, he has introduced legislation to better enforce state and federal “parity” laws, which require equal treatment of mental and physical health problems. Four times, that legislation has failed. As he enters his final year in the Legislature, the San Jose Democrat plans what he calls a “full-frontal assault.” “I’m going to put even more effort into next year,” Beall said, “because I’m madder than hell about it.”
California’s parity mandate was signed into law in 1999, and a federal version of the law followed in 2008. But the state has struggled to ensure those policies work‚ which helps explain why parity feels like an empty promise to so many Californians. More than half of state residents believe that most people with mental health conditions can’t get the services they need, according to a poll conducted last year by the Kaiser Family Foundation and the California Health Care Foundation.
Those who do get services often have to search hard and pay extra for them: California patients were more than five times more likely to have office visits for mental health or addiction problems from providers outside of their insurance plan’s network than patients seeking medical or surgical care, according to a new analysis by healthcare consultants Milliman Inc. Insurers here paid primary care providers 15 percent more than they paid behavioral health providers.
“We need stricter enforcement of mental health parity laws,” Gov. Gavin Newsom declared during his campaign. That didn’t happen again this year, although Dr. Tom Insel, Newsom’s top mental health advisor, recently said the administration intends to take “a fresh look at parity enforcement.”
“Instead of doing this topic by topic, let’s step back and find an overall plan, a blueprint, that tells us what’s the system we want,” Insel said in an interview. “I don’t think the state’s done that for a long, long time.”
What the state has been doing: rebuffing many attempts to tighten parity enforcement.
The most recent failure: Beall’s 2019 bill to ramp up requirements for health plans to report parity compliance data to state agencies each year instead of every three years, as it does now. The bill would have required the agencies to report results to the Legislature, and to post them on their websites to make them easily accessible to the public.
Beall said that would help make the state less reliant on patient complaints to trigger enforcement. The bill also would have prohibited insurers from requiring prior authorization and “step therapy”— or making patients first try lower cost medications before receiving other prescriptions to treat substance abuse.
With a public desperate for better mental health services, what is keeping the state from ensuring that health insurers and plans comply with state and federal parity laws?
Some note the lack of the kind of broad, emotionally affecting campaign that has moved the needle in other states. There’s also disagreement among mental health advocates about whether Beall’s proposals would best address the problem.
The senator, for his part, has another explanation. “The insurance companies have too much power in Sacramento on the subject of mental health,” he said. “Whatever support I’ve gained has been countered by them effectively. ... They’re the best lobbyists in Sacramento that money can buy.”
Industry reps maintain that a crackdown is needless, saying the real challenges relate not to compliance but to a well-documented statewide shortage of mental health providers. “Health plans in California have made mental health a top priority, going above and beyond what the mental health laws are requiring,” said Mary Ellen Grant, spokeswoman for the California Association of Health Plans.
Many plans are putting behavioral health providers in primary care offices and using more telemedicine, she said. “We’re not aware of any legislation that would improve whatever it is that Senator Beall thinks is the issue,” she added.
Leanne Gassaway, a senior vice president for America’s Health Insurance Plans, warned “there will be 50 different flavors of auditing and reporting” if each state creates its own parity reporting tool. Instead she recommended the federal government create a single one. “We don’t have a problem with reporting,” she said.
States aren’t asking the right questions or getting granular enough data, said Dr. Henry Harbin, former CEO of the behavioral health care company Magellan Health. The result: California’s approach “has not produced the change you would expect it to have.”
Once a problem is identified, is the state doing enough to enforce it?
Beall doesn’t think so, and neither does Meiram Bendat, a Los Angeles lawyer and psychotherapist who won a much-touted case this past spring. In that lawsuit, a Northern California federal court found that United Behavioral Health had wrongly restricted treatment for patients with mental and substance abuse disorders in order to cut costs.
Bendat said that, over the years, many patients had asked the state Department of Managed Health Care for help with mental health claims denied by United Behavioral Health. But he said the department, which oversees health plans that receive monthly fees to provide health care for their members, has failed to inform the public of any systemic, corrective action against the insurer. He uses the terms “toothless and ineffective” to describe the department’s parity enforcement.
California allows plans to decide, for themselves, what makes a treatment “medically necessary” based on clinical standards. Critics, such as Bendat, contend plans often apply the wrong standard of care. Some other states require the use of medical necessity criteria determined by non-profit, clinical specialty organizations.
“California is behind the curve in this regard,” Bendat said. “The abuses that we see by managed care are widespread and ruinous and they need to be stopped,” he said.
Bendat and others do praise the work of the Department of Insurance, which covers a small fraction of the state’s health plans.
The Department of Managed Health Care wrote in an email that it “works diligently to ensure that health plans comply with state and federal requirements regarding mental health services.” This includes surveying all licensed plans every three years, interviewing plan staff, reviewing enrollee files, and tracking complaints.
In recent years, the department reports that it added two staff members and conducted focused comprehensive reviews of 25 health plans’ methodologies for providing mental health services. It then required those plans to eliminate impermissible day and visit limits, revise prior authorization requirements, and reimburse enrollees a total of more than $517,000. In the last decade, it has cited health plans dozens of times for mental health-related violations, resulting in more than $4 million dollars in fines—most levied against Kaiser six years ago.
The department said if patients feel they have been denied medically necessary treatment by their health plans, they can appeal to the state for an independent medical review. But critics say the vast majority of patients never appeal.
Sen. Beall expressed outrage over the swelling numbers of untreated individuals residing under doorways and overpasses. “It sounds horrible, doesn’t it?” he asked. “That’s because that’s what it is. It’s a horror.”
Beall was an undergrad studying urban planning and political science at San Jose State in the early 1970s, when Gov. Ronald Reagan began shuttering the state’s mental hospitals at the same time traumatized veterans returned from Vietnam. Years later, as a Santa Clara County Supervisor and liaison to the county mental health commission, Beall said he learned how mental health and substance abuse impacted all corners of society: housing, criminal justice, health, education, foster care.
“We kept seeing people ending up in our system because private insurance wouldn’t cover them adequately,” he said.
After Beall was elected to the Legislature in 2006, he began trying to pass laws to strengthen mental health parity. One made it through the Assembly and died in the Senate. Another made it through the Senate and died in the Assembly. A third, which would have allowed additional penalties of $2,500 per patient per day for each parity violation, was vetoed by Gov. Jerry Brown, who said the state insurance commissioner already had “broad authority” on enforcement. The most recent bill never left the Senate.
“I’m in a lot of pain right now. It hurts,” Beall said at a Sacramento forum on mental health organized by CalMatters, a few days after the latest bill died. He has spoken publicly in the past about having a family member with schizoaffective disorder. “I tried four times and it’s actually getting harder to get it passed. … My own colleagues killed it.”
The industry has opposed parity laws for a long time. Health insurers “fought tooth and nail” against California’s state parity law, stopping it twice in the 1990s before it ultimately became law, said the law’s sponsor, former state Assemblywoman Helen Thomson of Davis. A psychiatric-nurse-turned-legislator, she said the law was eventually pared back to cover just nine serious mental illnesses because of this pushback.
In the case of Beall’s most recent bill, he said he had to remove the parity provisions because members of the Senate Health Committee disagreed with them. He also insists that some of his colleagues are too connected to health insurers, allowing ex-staffers and legislators who work for the industry to use those relationships to stop his bills.
In the years that Beall has been trying to pass parity legislation, health insurers have contributed almost $10 million directly to winning candidates and industry lobbyists have spent more than $85 million.
Other states did pass parity-related bills last year, among them Colorado, Connecticut, Delaware, Illinois, New Jersey and Tennessee. A massive publicity effort featuring compelling personal stories, combined with negotiations, may be part of the equation—and part of what’s been missing in California. Often, health insurers dropped their opposition after intensive negotiations and media and education campaigns, said Tim Clement, director of legislative development at the American Psychiatric Association,
Clement, who was at the negotiating table in many of those states, but not California, called it “pretty close to impossible to get a bill passed if insurance industry opposed.” He blamed California’s inaction partly on the lack of “a cohesive, boots-on-the-ground movement” for parity.
In Colorado—which just passed an expansive parity bill that will close loopholes, improve transparency and enforcement, and strengthen mental health prevention and screening—“we just were relentless,” said Lauren Snyder, state policy director with the advocacy organization Mental Health Colorado. That included working with media outlets to share personal stories of individuals harmed by lack of mental health care, and ads urging people to contact their legislators.
Such a movement was part of what eventually worked in California in the 1990s, said former Assemblywoman Thomson. She said she had a full-time public relations person working on the effort to pass a parity law, that major newspapers in the state editorialized in its favor, and that many legislators gave personal testimonies about how lack of mental health care had impacted their loved ones.
That law now has strong provisions for the coverage of medically necessary treatments for serious mental illnesses like schizophrenia and bipolar disorder, but does not cover a wide range of other mental health conditions or substance abuse disorders. Some parity advocates say California needs to ensure medically necessary treatment for more individuals, including those with substance abuse disorders.
Dr. Richard Pan, a Sacramento pediatrician who chairs the Senate Health Committee, wants to give plans more incentives to serve people with serious mental illnesses. “No one wants to be known as the health plan with the best mental health coverage or diabetes or asthma,” he said. His idea: a shared risk pool to reward plans that provide quality care for people with chronic conditions.
For a long time, Sen. Beall has “carried the mantle on (mental health parity), kind of alone,” said Sacramento Mayor Darrell Steinberg, a former state senate leader who founded the Steinberg Institute to advocate for mental health policies.
Beall called his inability to pass a parity law thus far “my biggest failure as a legislator.”
Earlier this year, the Assembly passed a resolution calling on relevant state agencies and the Attorney General to ensure that all health insurers are complying with federal and state parity laws. But a resolution, while it may raise awareness, is akin to a suggestion.
Beall said he’d like to introduce one more parity bill before he terms out—though he’s still working out the details.
“My style is to keep fighting and fighting and fighting,” he said. “I don’t give up.”
Jocelyn Wiener is a CalMatters contributing writer. Her reporting is made possible by a grant from the California Health Care Foundation. CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.

> CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
So, CalMatters wants to explain California policies and politics to ME!
To little old ME!
How thoughtful of them. What a great bunch of guys!
AND . . . they’re non-partisan, and not tainted by lust for profits. What could be better?
Maybe since they’re so helpful, and unbiased, and public spirited, they could cast our ballots for us instead of having to go through all the rigamarole of getting the public to vote.
It would certainly increase voter participation (one hundred percent!) and probably better government since all the voting would be done by informed experts who just care about good government.
when will this blow hard retire?